When people refer to Human Immunodeficiency Virus (HIV), the virus appears to be singular, but it’s a lot more complicated than that, as there are two types of HIV that branch out into different groups, subtypes and strains. As I have described in previous articles, HIV is very sophisticated, as it has figured out how to replicate inside the human body so it can survive and multiply over time, at the cost of our immune system. This article will introduce you to the variations that make up HIV and even though discussions involving HIV can often be complicated and scientific, this article will explain things as simply as possible.
Different Types of HIV
There are two types of HIV, with HIV-1 being the most common type of HIV that accounts for approximately 95% of all infections worldwide. HIV-2 is less common and is primarily found in West Africa, but it has also been identified in some other countries including India, Portugal, France, United Kingdom and the Americas, mainly in individuals with links to West Africa. HIV-1 is more infectious and the virus progresses faster, whereas HIV-2 is less infectious and the virus progresses more slowly.
Both types of HIV might sound similar, but HIV-2 is more than 55% genetically different from HIV-1. There are HIV tests available that are sensitive to both types of viruses, but only one antibody test is currently approved by the U.S. Food and Drug Administration (FDA) to distinguish between antibodies to HIV-1 and HIV-2, which is the Multispot HIV-1/HIV-2 Rapid Test. Many commonly used antiretroviral drugs work against HIV-2, but non-nucleoside reverse transcriptase inhibitors (NNRTIs) do not work against it, so regimes based on an integrase inhibitor or protease inhibitor are recommended by healthcare professionals to treat HIV-2.
Groups with HIV-1
The different strains of HIV-1 can be classified into four groups, with them being Group M, Group N, Group O and Group P. Group M is the strain of HIV that is responsible for the global HIV epidemic and the letter M stands for “major”. The other three groups are fairly uncommon, with Group O representing 5% of infections in several west and central African countries and Group N and Group P have been occasionally identified in Cameroon. Group N stands for “non-M, non-O”, Group O stands for “outlier” and Group P stands for “pending the identification of further human cases”. All groups within HIV-1 can be detected by HIV-1 antibody tests.
Subtypes within HIV-1 Group M
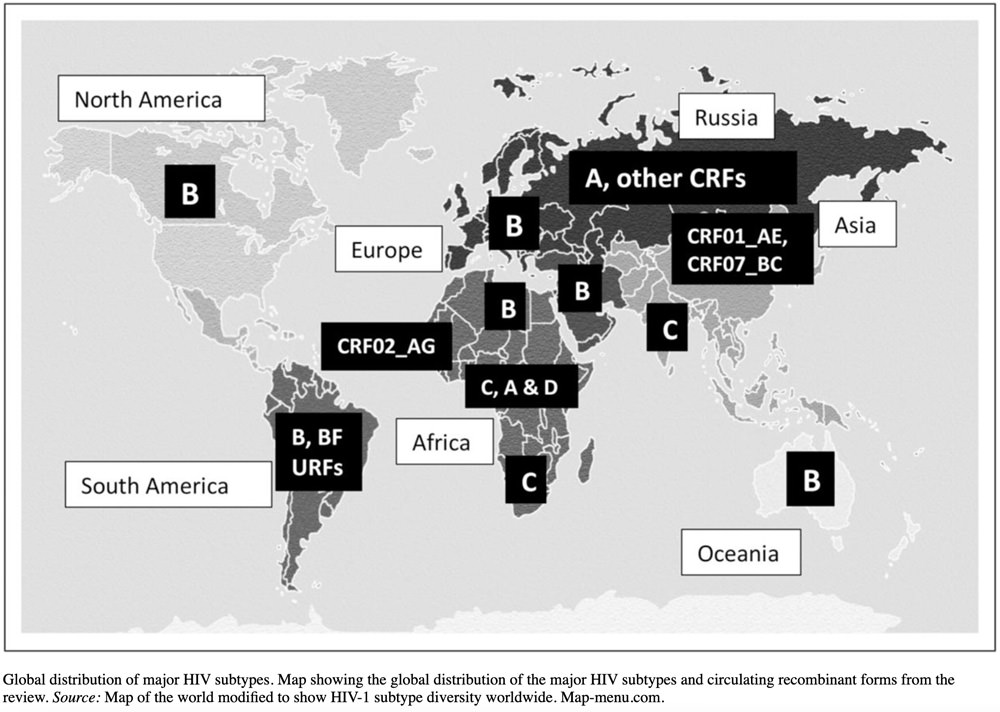
If you look more closely at HIV-1 Group M, there are at least nine genetically distinct subtypes of HIV-1, which are subtypes A, B, C, D, F, G, H, J and K. If you noticed that the letters E and I are missing from this list, there is a reason and you will find out why below. To complicate things a little further, different subtypes can combine genetic material to form a hybrid virus, which is known as a “circulating recombinant form” or CRFs and around 89 of these are known to exist.
The dominating HIV subtype in the Americas, West Europe and Australasia is subtype B, which has resulted in the majority of research relating to subtype B, even though this subtype on represents approximately 12% of global HIV infections. Less research is currently available for subtype C, which accounts for approximately 47% of people living with HIV, which has a higher prevalence in South Africa and India and subtype A common in eastern Africa is responsible for approximately 10% of infections. The greatest diversity of subtypes can be found in Cameroon and the Democratic Republic of Congo, which is the region where the HIV-1 epidemic originated, although with population mixing, the distribution of subtypes can change over time.
| SUBTYPE | LOCATION |
|---|---|
| A | Common in eastern Africa. |
| B | Dominant form in Europe, the Americas, Japan, and Australia. In addition, subtype B is the most common form in the Middle East and North Africa. |
| C | Dominant form in Southern Africa, Eastern Africa, India, Nepal, and parts of China. |
| D | Generally only seen in Eastern and central Africa. |
| E | Was originally used to describe a strain that is now accounted for as the combined strain CRF01_AE. This means the original, singular, E strain has disappeared, but scientists know it existed, as it is visible in this combined strain form. |
| F | Has been found in central Africa, South America and Eastern Europe. |
| G | This subtype and the strain CRF02_AG have been found in Africa and central Europe. |
| H | Is limited to central Africa. |
| I | Was originally used to describe a strain that is now accounted for as CRF04_cpx, with the cpx meaning a “complex” recombination of several subtypes. |
| J | Primarily found in North, Central and West Africa, and the Caribbean. |
| K | Is limited to the Democratic Republic of Congo (DRC) and Cameroon. |
Infections with Multiple Strains
If you are wondering whether you can be infected with different strains, the answer is yes. When the virus replicates, the copies can sometimes change, as the virus doesn’t always create an identical version of itself using its genetic material, which is referred to as a virus mutation. These mutations develop into another HIV strain, so it’s possible you can have various strains in your body and there’s the risk that HIV drugs won’t work against them. If this happens, your CD4 count will reduce and your viral load will increase, so other treatments will need to be investigated, as without treatment, the virus will progress to AIDS and can result in a life-threatening outcome. You can also have two or more strains if you were infected by more than one person, which is referred to as superinfection. Everyone reacts differently to infection, so there may be no noticeable difference in symptoms or viral load with a new infection, or it could be the opposite.
If you live in Australia, Canada, Europe, the United Kingdom or the United States, you will most likely have HIV-1, Group M, Subtype B. If you live in a different region, you will also most likely have HIV-1 and Group M, but your subtype might be different based on the list above. You may have also heard about the Cuban strain (CRF19) that was discovered in 2015, which is a combination of subtypes A, D and G, which can develop into AIDS within 3 years instead of the usual 5 to 10 years, as this strain does not respond to most antiretroviral drugs. With population mixing, this is just a general guide and it’s possible to contract a different variation of HIV, so this information, as with everything published at this website, must be used for general information only.
Sources and Further Reading:
- HIV-1 and HIV-2 – https://www.aidsmap.com/about-hiv/hiv-1-and-hiv-2
- HIV Circulating Recombinant Forms (CRFs) – https://www.hiv.lanl.gov/content/sequence/HIV/CRFs/CRFs.html
- HIV subtype diversity worldwide – https://journals.lww.com/co-hivandaids/fulltext/2019/05000/hiv_subtype_diversity_worldwide.3.aspx
- How Many HIV Strains, Types, and Subtypes Are There? – https://www.healthline.com/health/hiv/hiv-strains
Featured Photo: Gerd Altmann from Pixabay.
Article ID: CC025
Version Control: 1.0 – January 18, 2022: Original article published.



One guy told me that since HIV mutates so quickly and so much, that pretty much everyone’s virus is unique. There’s a new HIV variant that was discovered in the Netherlands. https://globalnews.ca/news/8595861/new-hiv-strain-discovered/
I’ve read about it and discovered the same thing about its potency. Not sure if it’s that prevalent in Cuba or not lol but as something else to chase it is very tempting.
As I remembered from my science classes, I knew viruses can mutate (ever so slightly) every time it encounters a host and replicates itself, so I knew that HIV was not a “singular” virus now. What I did not know is all of the subtypes of HIV. I find this extremely fascinating! What I find erotic is that a gifter’s HIV virus will quite likely take DNA material from the receiver and use it to create a slightly mutated version. Thus, becoming a “product” of both the gifter and receiver, so the term HIV “babies” is truly more accurate than most think.
Thanks, Jason, for this article and the website!
Thank you for this illuminating article which explains not only the strains and types of hiv infection but where and why. I have read similar articles which only left me scratching my head. This one left me fondling my balls instead.
Profoundly grateful for every enlightening resource your articles. Your dedication and devotion to bring informative awareness, convey a positive conversation towards HIV and Bug Chasing.
Wow! Great information – thank you.
Another educational article! Thanks for all the work you do!
I heard that the Cuban strain of HIV is the deadliest.